The Leva Therapy Advantage for PFMT
Supervised pelvic floor muscle training (PFMT) is globally recommended as part of first-line treatment for UI8 and proven to work, but most women don’t perform their exercises correctly, or at all.9
Backed by science,
Clinically Proven: Leva Therapy Outperforms Traditional Pelvic Floor Treatments
Clinical data supports the use of Leva for patients with stress, mixed, and urgency UI, including overactive bladder. In our randomized controlled trial with 299 women, the Leva group achieved significantly greater improvement on both primary endpoints vs. the at home pelvic floor muscle training group.1
3 day bladder diary:
Leva users reported significantly fewer stress UI episodes at 8 weeks
UDI-6 scores:
Leva users achieved significantly greater UI symptom improvement at 8 weeks
Improve Your Patients’ Pelvic Health With Leva
Leva offers a modern and convenient way to deliver supervised pelvic floor muscle training.

01: Leva Device
Inserted vaginally, the flexible Leva wand is embedded with motion sensors along the length of the device that detect movement during pelvic floor muscle training.

02: Leva App
The sensors communicate with the smartphone app that gives the patient real-time visual feedback and guides women through therapy.

03: Leva Women’s Center
The Leva system is supported by the Leva Women’s Center which is a team of educators & coaches dedicated to helping patients with their training, ongoing adherence support and reaching their personal symptom goals.

04: Leva Patient Reports
The patient report captures adherence and symptom data which is shared securely with you, so that you are able to remotely monitor patient’s progress over time.
Meet Our Experts

Samantha J. Pulliam, M.D., FACOG, URPS
Chief Medical Officer
Dr. Pulliam joined Axena Health in 2023 bringing with her a breadth of experience in Women’s health, including a successful academic and clinical career. Dr. Pulliam joined Axena because of her passion for helping to treat the 20 million women, in the U.S. alone, experiencing urinary incontinence, using technology with proven effectiveness. Dr. Pulliam oversees Axena Health’s clinical research program.
Dr. Pulliam was previously the Chief Medical Officer at Renovia, Inc., where she directed clinical research, including the successful completion of an all-remote clinical trial using Leva during the global pandemic. She was the Division Director for Female Pelvic Medicine and Reconstructive Surgery (FPMRS) at UNC-Chapel Hill and Associate Director FPMRS at Massachusetts General Hospital in Boston, and she was past Council Chair for the American Urogynecologic Society (AUGS) and remains active in the AUGS grants program.
Dr. Pulliam received her Bachelor of Science degree in Biology from Duke University and her Medical Degree from Wake Forest University School of Medicine. She completed residency training at Brigham and Women’s Hospital, and Fellowship training at Mount Auburn Hospital in Boston. She is board-certified in Obstetrics and Gynecology and FPMRS.
Dr. Pulliam’s favorite quote is: “Only those who will risk going too far can possibly find out how far one can go.” T.S. Eliot.

Jessica McKinney, PT, DScPT, MS
Vice President of Clinical Affairs and Global Health
Dr. McKinney joined Axena Health in 2023, bringing over 20 years of career experience as a women’s health care clinician, educator and advocate across high- and low-resource settings. With a deep commitment to health equity and career-long dedication to capacity-building in healthcare, Dr. McKinney joined Axena Health to pursue global access to care for women with incontinence through technology and clinical evidence.
Prior to Axena Health, Dr. McKinney served as a VP, Medical Affairs and Clinical Advocacy at Renovia, Inc. the medical device company who developed and first commercialized the Leva Pelvic Health System, and she was co-founder of Marathon Physical Therapy and Sports Medicine (Eastern Massachusetts) and Director of Marathon’s Center for Pelvic and Women’s Health. Her career has included over 10 years as faculty in the Female Pelvic Medicine and Reconstructive Surgery (FPMRS; Urogynecology) fellowship program at Mount Auburn Hospital (Cambridge, MA) and mentorship of physical therapy students and early-career professionals. Dr. McKinney also provides programmatic and research support in global health and development and has contributed to multiple peer-reviewed publications, abstracts and academic videos in the areas of pelvic pain, global and domestic maternal and female pelvic health, fistula, and surgical ergonomics and is a regular educator and speaker on these subjects.
Dr. McKinney’s favorite quote is: “When many little people in many little places do many little things, then the whole world changes, but sometimes not fast enough for me” from the song “Gloria” by Michael Franti.

Laura Keyser, DPT, MPH
Director of Clinical Strategy and Global Health
Dr. Keyser joined Axena Health in 2023 bringing over 15 years of experience as a clinician-leader and public health professional with expertise in women’s and pelvic health. She is a skilled researcher, writer, speaker, and educator with demonstrated professional competence in several key areas including maternal/women’s health, life course health development/health disparities, public/population health, digital health, capacity building and health care delivery models, with a focus on low resource and conflict settings. In the U.S. Dr. Keyser has worked with a women’s health company focused on digital health innovations for female pelvic floor disorders, contributing to product development and research efforts, including efficacy trials, real-world evidence generation, health economics work, and clinical decision-making tools. Her international experience includes women’s health and physiotherapy capacity building in India and multiple countries across Africa, with a focus on special populations, such as women with obstetric fistula, survivors of sexual violence, and pregnant/postpartum individuals. Dr. Keyser has published and lectured on her work in global and women’s health and consulted with local and international organizations, including EngenderHealth, USAID, Johnson & Johnson, Panzi Hospital & Foundation, and Global Strategies. She serves as an assistant clinical professor at the University of California, San Francisco, as co-founder of Mama LLC, and most recently as a founding member of Axena Health, Inc.
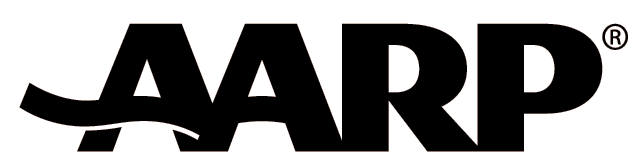
Get The Resources You Need To Treat UI
We offer valuable resources, for you, your practice, and your patients.
Recognized as a 2023 medical breakthrough in women’s health by AARP.