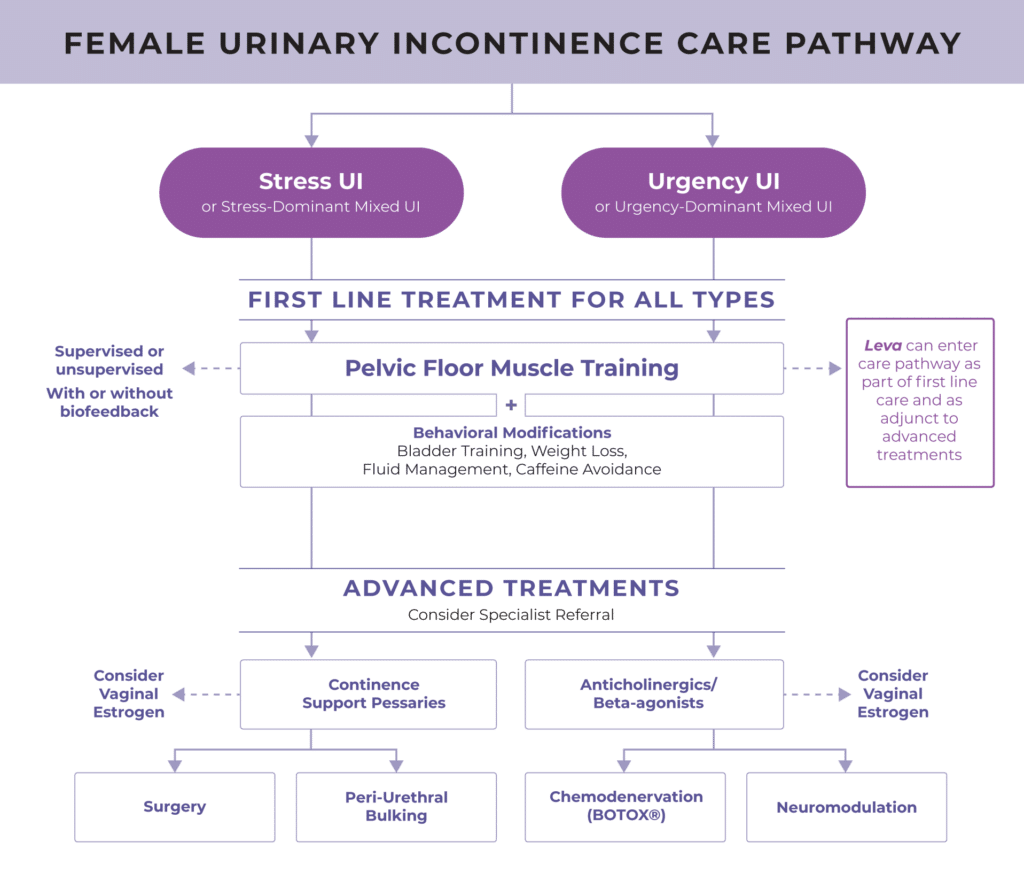
Recommended Care Pathway for Female Urinary Incontinence
Professional societies, including AUGS and ACOG recommend Pelvic Floor Muscle Training (PFMT) as first-line treatment for stress, urgency, and mixed UI. Findings from an overview of Cochrane Systematic Reviews further validate this, “There is high certainty evidence that undertaking pelvic floor muscle training can cure symptoms and improve quality of life for all types of urinary incontinence. There is moderate or high certainty evidence that these pelvic floor muscle exercises work better if they are more intense, have more support from a health care professional, and are combined with strategies to support continued use.“

Prevalence of Female Urinary Incontinence Increases with Age
Urinary incontinence (UI) is a growing epidemic, affecting 78 million women in the U.S. alone.1 Over 28 million women report moderate or severe UI symptoms,1 yet only about 11 million women seek treatment.2 According to market research, women wait an average of 6.5 years before they bring this up with you, their provider, if they even bring it up at all.3
And if nothing is done… UI may progress over time.
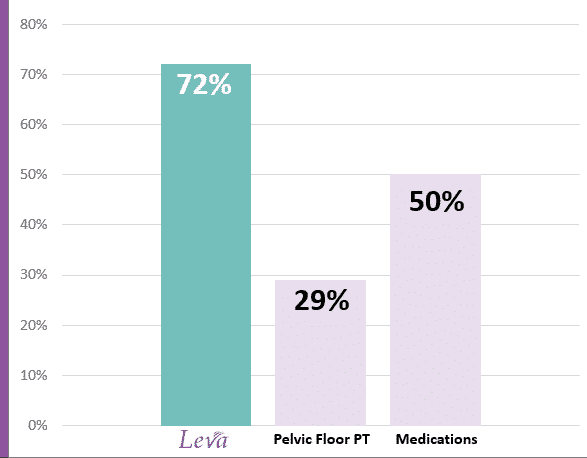
Typical Patient Adherence to Common UI Treatment Options
Leva Pelvic Health System (at-home pelvic floor therapy)
Among women prescribed Leva, women used Leva an average of 1.5x daily, or 72% of recommended uses.5
Pelvic Floor Physical Therapy (PFPT)
Of women who start PFPT, only 29% complete a course of care defined as three visits.6
Medications
Of women taking medications as prescribed, 50% discontinue use within five months.7
Recognized as a 2023 medical breakthrough in women’s health by AARP.